Goal
Given the limited large-scale, high-quality data on antibiotic prescribing in low- and middle-income country (LMIC) private, primary healthcare settings, this project uses large-scale healthcare surveys to assess antibiotic prescribing levels and the factors influencing prescribing decisions for common infections in these settings in Pakistan, Egypt, and Indonesia.
Lead
Nam Nguyen – Nuffield Department of Primary Care Health Science, University of Oxford
What we did
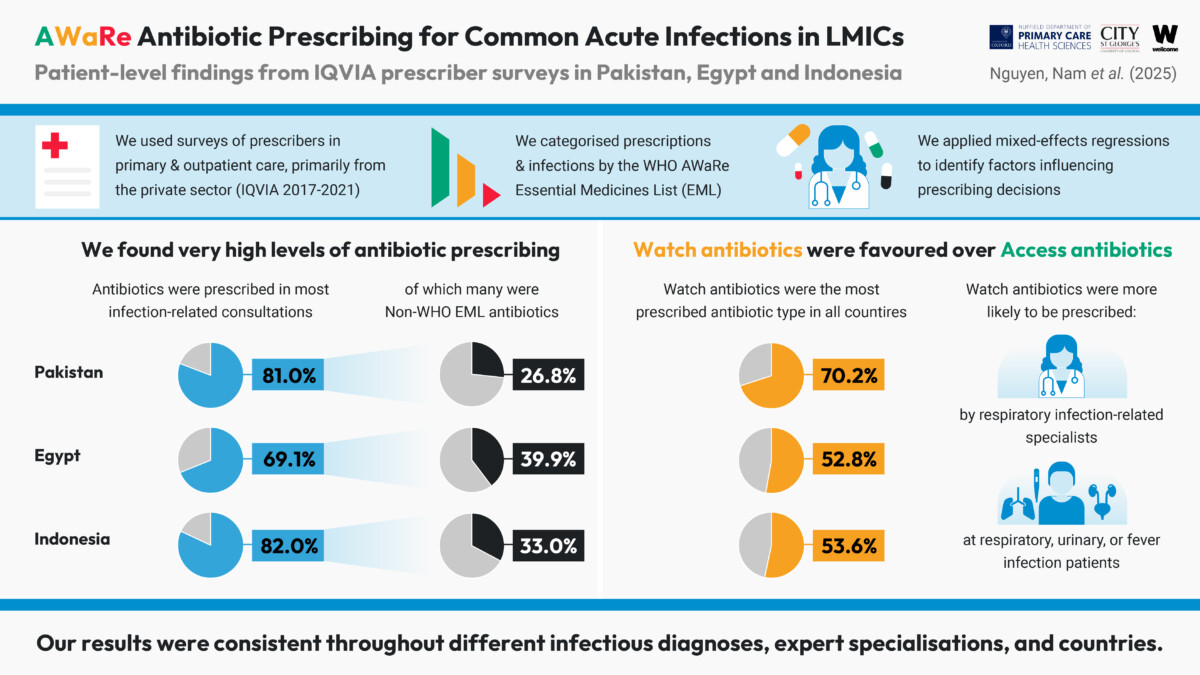
This project uses IQVIA-conducted healthcare surveys between 2017 and 2021 to assess antibiotic prescribing levels for common infections and the factors influencing prescribing decisions in Pakistan, Egypt, and Indonesia. We found that among the 384,975 infection-related health records analysed, antibiotics were prescribed in 82.0% of cases in Pakistan, 81.2% in Egypt, and 69.1% in Indonesia, with Watch antibiotics accounting for 70.2%, 52.9%, and 53.6% of prescriptions, respectively.
Key learnings
The study highlights routine antibiotic over prescription and the preferential use of Watch antibiotics over Access antibiotics for common infections, consistently observed across most medical specialties in all three countries. As both patient-level factors, such as specific infectious conditions and accompanying fever, and prescriber-level factors, including prescriber specialty, are associated with higher antibiotic prescribing and Watch antibiotic use, our findings suggest that future antibiotic stewardship programmes in LMIC private primary care should target both drivers.
Outputs
Funder
The Wellcome Trust

